Introduction
Cancer is one of the leading causes of death worldwide. By 2050, global cancer deaths are projected to reach 18.5 million, a staggering 90% increase from the estimated 9.7 million deaths in 2022. This is not surprising, given that 35.3 million new cases are predicted in 2050, a 77% increase from the estimated 20 million new cases in 2022. The rapidly growing global cancer burden is attributable to factors such as population growth, an aging population, and changes in exposure to risk factors like tobacco, alcohol, obesity, and air pollution. Therefore, regular cancer screenings – even in the absence of symptoms – play a crucial role for early detection and treatment, which can help to save lives. The goal of cancer screening is to reduce mortality and morbidity through early detection and early treatment of cancer (e.g., breast screening), or to reduce the incidence of cancer by identifying and treating its precursor before disease progression (e.g., cervical screening). The following are the screening recommendations for the general population by various health organizations, for cancers with sufficient scientific evidence of effectiveness.
Breast cancer
Guidelines recommend that all women should begin yearly screening with mammograms at age 45 until 54. From age 55 onwards, women can switch to biannual screenings or continue with annual screenings. Regular screenings should be continued as long as the woman is in good health and is expected to live for at least another 10 years. It should be noted that mammograms may not be suitable for women with dense breasts due to higher risk of false-negative results, although they are at a higher risk of developing breast cancer. For women with dense breasts, additional tests such as ultrasound, magnetic resonance imaging (MRI), digital mammogram, or digital breast tomosynthesis (DBT) may be considered.
Cervical cancer
Regular screening should start at age 21. Women ages 21 to 29 should get a Pap test every 3 years. The human papillomavirus (HPV) test is not recommended for women ages 21 to 29 because of the high prevalence of transient HPV infections in this age group. Women ages 30 to 65 should get a primary HPV test every 5 years. If a primary HPV test is not available, a co-test involving HPV combined with Pap test should be performed every 5 years, or Pap test every 3 years. Women above age 65 who have had regular screenings in the past 10 years with normal findings should no longer be screened for cervical cancer, although those with a history of serious pre-cancer lesions should continue to be screened for at least 25 years after that diagnosis, even if the testing goes beyond age 65. Importantly, women who have been vaccinated against HPV should still follow screening recommendations.
Colorectal cancer
Adults should begin regular screening at age 45 until 75. After age 75, regular screenings can be continued if they wish to do so. Several different tests are available for colorectal screening, with screening frequency depending on the preferred test. For example, stool examination for occult blood or immunohistochemical test (yearly), stool DNA test (every 3 years), sigmoidoscopy (every 5 years), computed tomography (CT) colonography (every 5 years), and colonoscopy (every 10 years). All abnormal findings with non-colonoscopy screening tests should be followed up with a colonoscopy.
Prostate cancer
Screening for prostate cancer involves making an informed decision due to its uncertain benefit. Men at age 50 and above should discuss the potential risks and benefits of screening with their doctors before deciding. The two main screening tests are prostate-specific antigen (PSA) blood test and digital rectal exam (DRE), with the frequency of screening depending on the results.
Lung cancer
Yearly screening with low-dose CT scan (LDCT) is recommended for high-risk adults between age 50 to 80. High-risk individuals are people who are smoking or have quit smoking, and have at least 20 pack-year history of smoking (a pack-year is equivalent to smoking 1 pack or about 20 cigarettes per day for a year).
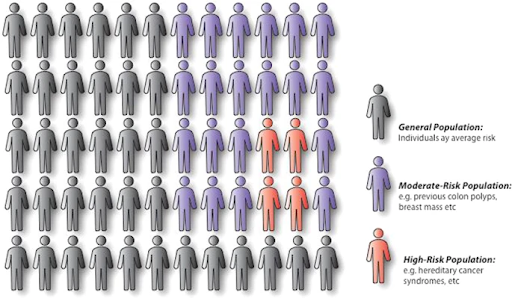
Regular cancer screening is a vital strategy in the fight against cancer by enabling early detection, timely intervention, improved treatment outcomes, and enhanced quality of life. While the recommendations above provide a general framework, they are not a one-size-fits-all model. Individuals at higher risk, such as those with a genetic predisposition, a strong family history, or a previous cancer diagnosis, may need to undergo screening more frequently or start at a younger age. Additionally, other screening tests not listed here may also be suitable. For instance, there is a growing interest in multi-cancer early detection (MCED) tests, which have the potential to detect multiple cancers earlier than traditional methods from a simple blood draw. Early findings from several ongoing clinical trials evaluating the performance of these tests show promising results. As these trials progress, some of these tests could eventually receive the necessary approval to be incorporated into standard cancer screening protocols. Therefore, it is important for individuals to discuss with their doctors which screening tests to undergo, when to begin, and the recommended frequency, so they can make an informed decision.
Canary Oncoceutics has a steadfast commitment to three fundamental pillars: advancing scientific knowledge, fostering collaboration, and ultimately, enhancing the lives of cancer patients worldwide. From cutting-edge research to impactful clinical advancements, Canary Oncoceutics aims to illuminate the transformative potential of tailored cancer treatments. Join us on this journey towards a future where every cancer patient receives personalized, effective treatment tailored to their unique needs.