Introduction
Radioligand therapy (RLT) represents a cutting-edge approach that combines the precision of a targeted approach with the potency of radiation. By utilizing a ligand to direct a concentrated dose of radiation to cancer cells, RLT delivers cancer treatment with high accuracy, sparing surrounding tissues from unnecessary harm. This innovative approach not only enhances the treatment efficacy, but also reduces the risk of adverse effects, leading to a better quality of life for cancer patients.
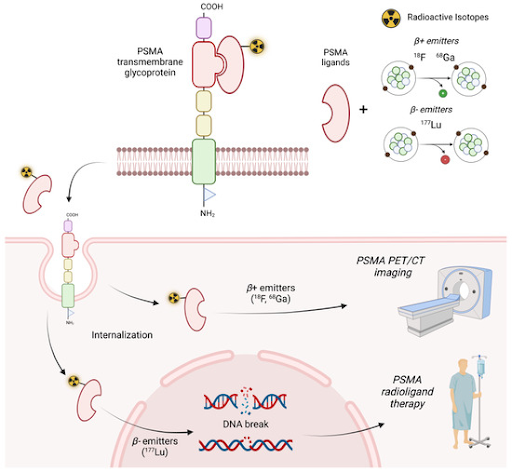
RLT delivers radiation with precision
RLT involves the use of specially engineered targeting molecules known as ligands, which can be antibodies, peptides, or small molecules, designed to have a high affinity for antigens or receptors expressed on cancer cells. These ligands are conjugated to a radioactive isotope (radioisotope) via a linker, serving as the therapeutic agent to kill the cancer cells. Once administered to the patient via an intravenous injection, the ligands seek out and selectively bind to cancer cells that display the targets. Upon binding, the radioisotope emits ionizing radiation such as alpha or beta particles to induce DNA damage and kill the cancer cells. Alpha emitters, with their shorter range and higher energy, are ideal for targeting small clusters of cancer cells. In contrast, the lower energy beta emitters are better suited for treating larger tumors due to their greater penetration range. Additionally, RLT utilizes a theranostic approach by using the same targeting molecule for both diagnosis and treatment to optimize therapeutic outcomes. First, a radiolabeled diagnostic agent is used to target specific antigens or receptors on the surface of cancer cells. This helps to confirm the presence of these targets and enables visualization of the tumor’s location, size, and extent using PET or CT scans. Following this, a radiolabeled therapeutic agent is administered to directly irradiate and kill the cancer cells.
The advantages of RLT over traditional therapies
One of the most significant advantages of RLT is its precision. Traditional radiotherapy can cause significant side effects due to its non-selective mechanism, although efforts are made to minimize collateral damage. In contrast, the targeted approach of RLT reduces the risk of affecting healthy tissues by delivering radiation directly to the tumor cells. Compared to the localized effect of traditional radiotherapy, where high energy radiation is directed at a visible tumor or a defined region, RLT offers a systemic approach, capable of targeting cancer cells anywhere in the body. This makes RLT an effective treatment strategy for metastatic cancers, where tumors have spread beyond the initial site. Additionally, RLT can exhibit a potent bystander effect due to the short diffusion distance of the emitted radiation. Therefore, the radiation not only affects the directly bound cancer cell but can also impacts neighboring cancer cells, even if they do not express the target antigen or receptor. This can be beneficial for overcoming tumor heterogeneity and enhancing overall treatment efficacy.
The challenges of RLT
Despite its potential, RLT is not without its challenges. Not all cancer cells within a tumor express the target antigen or receptor uniformly. If the tumor lacks a sufficient number of these markers, the radioligand cannot bind effectively, reducing the therapy’s efficacy. Thus, this heterogeneity can limit treatment efficacy and allow the tumor to persist, potentially leading to disease relapse. Another significant hurdle is the accessibility and availability of radiopharmaceuticals. The production of radioligands is a complex process that requires specialized manufacturing facilities, and the radioisotopes often have short half-lives. For example, the lutetium-177 used in prostate cancer treatment has a half-life of approximately 6.7 days. Although this is clinically advantageous, allowing sufficient time for the isotope to exert its anti-cancer effects while limiting radiation exposure to non-targeted tissues, it presents challenges in production and supply chain logistics. The relatively short half-life of the radioisotope means that it must be produced, transported, and used within a narrow timeframe. This can limit the accessibility of RLT, particularly in regions without specialized manufacturing facilities and reliable distribution networks. Additionally, the strict adherence to protocols required for handling and disposing of radioactive materials and waste can further hinder the widespread adoption of this therapy.
The promise of RLT in transforming cancer care
RLT marks a groundbreaking advancement in radiotherapy, enabling more precise and effective management of the disease. Several RLTs have already been approved for cancer treatment, including lutetium-177 vipivotide tetraxetan for treating prostate-specific membrane antigen (PSMA)-positive metastatic castration-resistant prostate cancer, and lutetium-177 dotatate to treat neuroendocrine tumors (NETs) that express somatostatin receptors on their surface. The field of RLT is rapidly evolving, with numerous clinical trials investigating new targets and expanding its potential across a wide range of cancers. Meanwhile, ongoing research is intensifying efforts to enhance the accessibility, precision, efficacy, and safety of this therapy. By delivering highly targeted radiation directly to cancer cells while minimizing the adverse effects commonly seen with traditional therapies, RLT is changing the landscape of traditional radiotherapy. This innovative approach promises not only to improve patient outcomes but also enhance their quality of life, marking a transformative shift towards more effective and personalized treatment strategies.
Canary Oncoceutics has a steadfast commitment to three fundamental pillars: advancing scientific knowledge, fostering collaboration, and ultimately, enhancing the lives of cancer patients worldwide. From cutting-edge research to impactful clinical advancements, Canary Oncoceutics aims to illuminate the transformative potential of tailored cancer treatments. Join us on this journey towards a future where every cancer patient receives personalized, effective treatment tailored to their unique needs.